Reading Civil War Medical Cases
A soldier stationed in the District of Columbia during the Civil War entered medical awareness when he reported to his regimental surgeon claiming illness or injury. At that moment, the surgeon composed a record, as it was his duty to make a daily report to his commanding officer on the number of men fit to serve. The medical record thus began as a practical military record: how many men can mount the defenses, march, make camp, and fight? The army then needed to keep track of men as they moved through the medical system, from regimental sick call to general hospitals, from initial event to recovery, return to duty, discharge, or death. The army had to issue pay to the sick and wounded and, if a soldier was discharged for medical reasons, to determine eligibility for pensions. This bureaucratic need for medical records laid the groundwork for the data that the Surgeon General's Office accumulated during the war. Surgeons' field and inspection reports, case notes, and pathological specimens added depth to the breadth of this data. After the war, the Surgeon General's Office processed over six million cases to create the Medical and Surgical History of the War of the Rebellion (MSHWR) seeking to transform this data into medical knowledge.1 Thousands of illustrative accounts of individual soldiers' cases then put flesh on the tables of numbers that fill the MSHWR's first volume.
Already I have used "cases" in two quite different senses. The first refers to the case as a data point, an entry in a field report or hospital register. The second refers to the case as a story, a narrative—even if a very short narrative—of a doctor's experience with illness, wounding, or multiple illnesses, multiple wounds, or even wounds combined with illnesses. Some soldiers made many data points, as they got sick and got well, were wounded and healed, or became sick and wounded and died. Others may have made just one data point, but survived long enough to become the centers of narratives that focused on the intersections between soldiers' bodies and the army medical system. We can read cases, then, at multiple moments in the records left behind.2 For this essay, a register for L'Ouverture Hospital, one of the military hospitals in Alexandria, provides the entrance point for reading cases as data points. Accounts about individual soldiers extracted from the MSHWR for hospitals in the District of Columbia and Alexandria offer the texts for reading cases as narratives. Both convey truths about medical experiences during the Civil War, but those truths are inevitably partial, fragmented, and at times frustratingly ephemeral.
L'Ouverture Hospital Register: Cases as Data Points
The register for L'Ouverture Hospital in Alexandria is both typical and unique.3 It is typical because physically it is the same as all printed registers distributed to general hospitals in 1864. It is unique because it was used in the only general military hospital in the Department of Washington created for black soldiers.4 Before L'Ouverture opened on February 15, 1864, African Americans in Alexandria had sought relief in a hospital run by Dr. John Reynolds Bigelow, who was nominally in charge of all health needs of the freed people of Alexandria. That hospital, according to Julia Wilbur, a member of the Rochester Ladies' Anti-Slavery Society who came to Washington to help the freedmen, regularly lacked needed supplies and was routinely neglected by Dr. Bigelow.5 As the number of black soldiers increased throughout 1863, the army decided that it needed a proper military hospital for them and established one with hospital tents set up around buildings on the corner of Prince and Payne Streets. Named after Toussaint L'Ouverture, the leader of the revolution that had freed the slaves in Haiti, the hospital opened with the transfer of sixteen civilian patients from Dr. Bigelow's Hospital (as it was called in the L'Ouverture Hospital register).6 The first soldiers arrived on April 26, 1864, and formed the majority of the 1,583 patients until it closed in September 1865, although some civilians continued to be treated there.7
The printed register itself defines a case by the content assigned to each column. A case at its most essential was a person moving through a hospital, tracked by dates of admission, discharge, transfer, or death. The small space allocated for "diagnosis" reduced the medical identity of the patient to the primary reason for entering the hospital, usually expressed in medical (erysipelas, acute bronchitis, neuralgia, hernia) rather than lay (old age, burn on face, mule kick, sunstroke) terms. Cause of death was equally laconic (tuberculosis, erysipelas, acute rheumatism, gunshot wound), if not simply absent.
The meager information allowed by the standard bureaucratic record barely acknowledges individuals. Yet, because each entry names a person, each line testifies to a human being suffering at a specific moment in time. Among the civilians, Frank Thompson, age 14, came into the hospital on February 15 with a gunshot wound to his right foot. He stayed for just over three weeks and "recovered, and was discharged." Pvt. Charles Jackson, 25, was admitted to the hospital from his regiment, the Thirtieth U.S. Colored Troops, with measles on April 26, 1864. He returned to duty five months later, clearly having been a very sick man. Pvt. Andrew Brown, 29, of the Twenty-Eighth U.S., was the first soldier in a long series of men entering from a field hospital with a gunshot wound on August 9, 1864, which he received in action outside the siege of Petersburg. He died August 11, with no cause of death given. When read as individual entries, cases in hospital registers are truncated narratives that raise unanswerable questions: How did a 14-year-old contraband get shot? What complicated Private Jackson's recovery from measles? Why did Private Brown die of his "flesh wound of [his] right leg" so rapidly, when Pvt. William Strawder, whose case followed immediately after Brown's, survived a "gunshot flesh wound of [his] right leg" and served until he was discharged on June 22, 1865?
Table 1. L'Ouverture Hospital register column headings
| Hospital Number | |
| Name | |
| Rank | |
| Co. | |
| Regiment | |
| Age | |
| When Admitted | |
| From What General Hospital Transferred | |
| From What Other Source Admitted: From field, from field hospitals, etc. | |
| Diagnosis |
| In Surgical Cases Only | On What Occasion Wounded—Date |
| Nature of Missile or Weapon. Round or conical ball, solid shot, bayonet, sword | |
| Treatment: Amputation—Date of Excision—Date of Other operation—Date of Simple dressing |
| Result | Returned to Duty: Date |
| Transferred to V. R. C.*: Date | |
| Transferred to other G. H., State or City: Date | |
| Furloughed: Date | |
| Deserted: Date | |
| Discharged from Service: Date | |
| Death: Date | |
| Readmitted from Furlough or Desertion: Date | |
| Remarks. Here state cause of death, of discharge, or of transfer to V. R. C.* |
* Veterans' Reserve Corps
Source: National Archives and Records Administration, RG 94, Field Records of Hospitals, 1821–1912, Register 578.
While tantalizingly little may be learned about individuals from the cases written into hospital registers, as data points each entry contributes context to the others. Frank Thompson, Private Brown, and Private Strawder were among the 219 cases of gunshot wounds, or 13.8 percent of the 1,583 individuals in our dataset (see "L'Ouverture Hospital Register Data" on the Data page); another 81 were listed as wounded from other causes, for a total of 300 (18.9 percent) wounded. Twenty-five of the 219 men with gunshot wounds (11.4 percent) died in the hospital, the unlucky Private Brown among them, while 34 of the wounded (11.3 percent) died. Indeed, the odds of dying of measles (4 out of 16 cases, or 25 percent) were higher than dying of a gunshot wound among this particular group of men and women, of whom 17.6 percent died from all causes. All sorts of numbers may be extracted from the data. Which numbers are meaningful depends, of course, on the questions to be answered. By analyzing a comparable register for a white hospital in Alexandria for the same period, for instance, morbidity and mortality rates could be compared across races in order to test Margaret Humphrey's conclusions about the disparate health status of, and care provided to, black troops compared with white ones.8 Age profiles, too, could be elicited (among the civilians, the oldest patient was 86, the youngest was a baby), or lengths of stay could be studied to reveal how long it took for black soldiers to recuperate enough to leave or to have suffered enough on the path to death.
Cases as data points can also be linked to other data points. Men listed as entering from white hospitals—among those listed as sources of admission were Armory Square, Judiciary Square, Finley, Auger, and Lincoln—could be tracked in those hospitals' registers to see how long sick and wounded African Americans were allowed to stay in them before being sent to L'Ouverture, assuming that these men were acknowledged as patients in the white hospitals at all. Matching names of emancipated slaves from the petitions filed under the District's Compensated Emancipation Act of April 1862 with those in the hospital register could suggest how many men went from slavery in the District to military service, and from service to sickness, wounding and death.9 Enmeshing individual hospital cases into larger networks of relationships, especially when the networks are so clearly located in space (Alexandria) and time (mid-February 1864 to the end of September 1865) might add texture to our understanding of the black experience of the war on the fringes of the nation's capital.
Civil War hospital registers have limitations as sources that will be familiar to anyone who has tried to find individuals in historical records: variations on the spelling of names; inadvertent errors in dates of admission, discharge, or death; and inexplicably blank table cells. There are significant constraints, too, on the interpretations that can be built on qualitative or quantitative analysis of this data, especially given the brevity of the diagnoses upon admission. Almost as many men entered with rheumatism (217) as came in with gunshot wounds (219), for instance. "Rheumatism" speaks to joint pain serious enough to disable soldiers, but is far too vague a condition to be mapped onto twenty-first-century diseases. "Gunshot wounds" may correlate more directly with physical conditions that make sense in twenty-first-century terms, but even those need to be understood as consequences of having been hit by a mid-nineteenth-century bullet fired by a midnineteenth-century handgun, musket, or rifle.
Reading cases in hospital registers gives us sick and wounded individuals inextricably linked to their fellow data points at very specific times and places. We can have no idea how accurate or complete the entries were, nor can we understand the medical labels applied as diagnoses without some immersion in mid-nineteenth-century medical texts. What we read is frustratingly brief. They nevertheless carry the authenticity—as fragile as that is—that comes with opening original archival sources. Whatever else these cases are, they speak to human experiences of suffering that are both universal and elusive.
Reading Cases 2: Narratives of Trauma and Disease
In 1875, Walt Whitman decided to publish an account of the Civil War as he experienced it, basing his work on the notes that he had scribbled while "watching, or waiting, or tending somebody amid those scenes" of sick, wounded, and dead soldiers in Washington and in nearby field hospitals. In his Memoranda during the War, Whitman offered fragments of moments in the wards, here sitting at the bedside a dying soldier, there giving treats to men who had no one else to comfort them. He described the wounded—"A bullet had shot him right through the bladder, hitting him front, low in the belly, and coming out back"—and the sick—"typhoid fever, pretty bad"—as metonyms for the suffering of the entire nation during the war. The three years spent "in Hospital, camp or field" gave Whitman "the perusal of those subtlest, rarest, divinest volumes of Humanity, laid bare in its inmost recesses, and of actual life and death. . . . It arous'd and brought out and decided undream'dof depths of emotion." Yet, even though Whitman's narrative evokes the presence of the sick and wounded, it is not really about them. It is about Whitman, his search for the meaning of the war, and his need to remind others of its human costs.10
Like Whitman's notes, the cases narrated in the Medical and Surgical History of the War of the Rebellion are not really about the sick and wounded soldiers. Compiled from a range of sources by each volume's editors, the cases are doctors' attempts to make sense of the traumas and diseases that soldiers' bodies presented to them and to construct medical knowledge out of the millions of discrete medical events they collectively faced.11 These accounts are deeply embedded in the medical theories and practices of mid-nineteenth-century America.12 As such, they can be disconcerting for the twenty-first-century reader, because many of the premises about wound healing, disease causation, and the efficacy of drugs remain implicit. The authors aimed their work at a medical audience presumably familiar with contemporary medical vocabulary and all that those words entailed about a basic knowledge of anatomy, physiology, pathology, and pharmacology in the 1860s and 1870s. By the time that the final volume was published in 1888, the emergence of bacteriology had begun to fundamentally alter theories about the causes and transmission routes of infectious diseases and to reshape understanding of wound infection and how to deal with it.13 The shifting directions of science thus left much of the MSHWR behind. And it is in that past that our Civil War cases reside.
Sometimes the case reports provide only bare documentation:
Ells, William S., Private, Co. K, 9th New York Cavalry. Sabre-cut of the scalp and right arm. Culpepper, Virginia, August 1st, 1863. Admitted to Douglas Hospital, Washington, August 3d. Returned to duty October 10th, 1863.14
Such terseness belies its significance: there was nothing unusual about this case to remark upon except that it happened. For the doctor, this soldier was wounded badly enough to have been transported to a general hospital in DC. He healed and was ready for duty in nine and a half weeks—business as usual. He was one of many whose sabre wounds were such uncomplicated injuries that they provided no interesting medical facts at all. Private Ells's case in the MSHWR could even have been transcribed directly from a hospital register.15
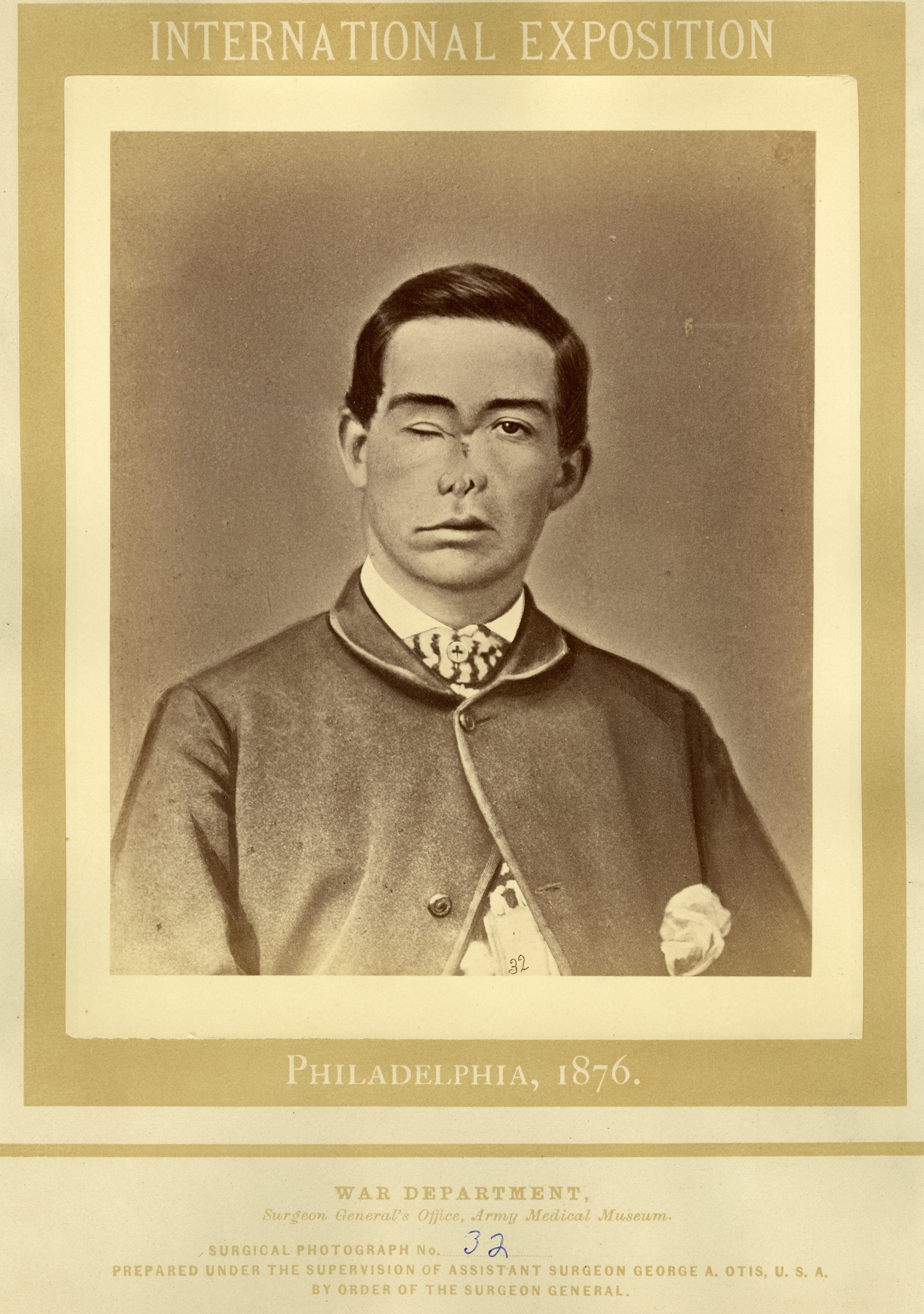
In contrast, consider the case of Pvt. William H. Nims, whose wound and treatment were more intriguing. The narrative conforms to a well-established format for describing medical cases.16 It begins with the essential identifying details of the sick or wounded person, which, for these Civil War compilations, meant the soldier's name, rank, regiment, and reason for coming to medical attention. Nims's reason was his encounter with "a fragment of shell" while fighting near Petersburg on June 17, 1864. The next phase of the story takes Nims from the battlefield to the hospital where most of the clinical observations took place. Nims first stopped in the field hospital of the First Division of the Second Corps and then was "sent to Columbian College Hospital." This journey took five days, which are passed over unremarked, although it was doubtlessly excruciating for Nims himself. Then began the important work of describing the patient's condition upon first examination: the "fragment of shell" had "evacuated the humors of the right eye, and fractured the nasal bones and right superior maxilla." This technical anatomical language brought precision to the injury: Nims's right eye had been punctured, his nose severely broken, and his upper jaw on the right side cracked apart. Enter the surgeon himself, Thomas R. Crosby, USV, who moved to act. Crosby first directed the treatment (removing bone splinters, bringing the edges of the gaping skin together), then took a hand with further operative skill, removing more dead bone and trying to get a scar to form to close the wound.
Then the denouement. Nims survived his injury and was discharged from service after having a photograph taken of his face for preservation in the Army Medical Museum (see Figure 1). In some survivors' cases, discharge or return to duty ended the story. In many, such as this one, a report from a pension examiner extended the drama. Here the case departs from the typical medical narrative, in that the volume editors included a compassionate comment about the injury. Nims, G. W. Avery reported in 1867, "continued to suffer greatly," and he could not work due to his "unpleasant deformity." "Thus," our narrator continued, "his mutilation was a doubly cruel one." Not only did Nims bear the marks of his wounds, as so many soldiers did, but he also was deprived of his independent manhood by the way that his face looked. We do not know what Nims thought about his experience, his traumatic wounding, his time at Columbian College Hospital, his pain during treatment, or his dreadful scarring. What Nims thought of his experience is absent because this was not his story. It was the doctors' story, even when one of the doctors wrote openly about Nims's suffering instead of dispassionately assessing his continuing eligibility for a pension. From the perspective of the Civil War surgeon, moreover, this was a good story: the soldier survived due to medical skill.
Many soldiers did not survive, of course. Case narratives offered multiple ways to understand the path to death. Pvt. John Lower, for example, entered Douglas Hospital on February 6, 1865, "with pain in the right side and cough of several weeks duration. He improved under treatment until March 1, when, having imprudently exposed himself, his symptoms became aggravated."17 Lower died, without even as much as a diagnosis, on March 25. It takes some familiarity with nineteenth-century medical prose to know that Lower had "exposed himself" to outside influences (likely cold, damp air), not that he committed an indecent act, and in doing so hastened his demise. Embedded in this simple statement is a world in which the interactions between the environment and the body produced illnesses through cold and heat, excessive damp, poorly cooked food, hideous smells from decaying organic matter, swamp vapors, and a host of other conditions in which the existence of microorganisms played no part at all. Such causes had explained epidemic diseases and various fevers since the time of Hippocrates, if not before.18 In this world, responsibility for proper precautions against such factors meant the difference between life and death, as Lower discovered.
Lower's story continued with his decline, delirium, and death. It did not end there. This case exemplifies another important characteristic of these medical narratives: they often continued after death, with the protagonist carrying on as a corpse. The drama moved inside the body, and narrators described the postmortem condition of flesh altered by diseases and weapons. In the 1860s the postmortem was the quintessential act of medical science at the bedside. The medical autopsy had become the laboratory for serious investigation of disease by elite physicians and surgeons in the mid-eighteenth century, but came into its own as a central investigative tool in the 1810s to 1840s, particularly as championed by practitioners in France.19 Linking clinical symptoms with pathological changes in organs and tissues had led doctors to add postmortem appearances to disease definitions. Tuberculosis of the lungs, for example, manifested as a cluster of clinical symptoms (weight loss, fever, chills, fatigue, cough—especially a cough that produces blood) that remained hard to pin down until physicians saw that some people with those symptoms had tubercles (nodules with dead tissue at the center) in their lungs when investigated at autopsy. The distinctive breath sounds that such tubercles produced in the living could be heard with the stethoscope (invented by Laennac in Paris in 1816) and allowed doctors who were trained in the use of this instrument definitively to diagnosis tuberculosis much earlier in its clinical course than doctors could in previous centuries.
It is thus not surprising that quite a few Civil War doctors continued their case narratives beyond their patients' deaths whenever they could, as they sought to verify premortem diagnoses, to understand why some wounds turned fatal, and to refine correlations between clinical symptoms and visible pathological lesions.20 The diarrheal diseases that plagued camp and field life particularly engaged the MSHWR editors, who sought to categorize them into diagnostic groups in order to get a grip on causal and therapeutic patterns.21 Typhoid, for example, which could cause diarrhea, was relatively easy to diagnose when patients developed a characteristic rash of flat dark pink spots, but could only be positively identified postmortem, after seeing specific kinds of ulcers in the small intestine.22
Narration of autopsies, like the narration of the case during the life of the patient, ranged from laconic one-sentence statements to lengthy disquisitions on the appearances of both healthy and diseased organs.23 Although the autopsy had become a central research tool by the Civil War, no agreed-upon format had emerged to structure either the practice or the subsequent written descriptions. Thus the case of Henry Clark, who suffered a fractured skull from a musket ball, simply ended with "The autopsy revealed the ball in the middle lobe of the brain."24 The author of the case of Private Otis G—, in contrast, noted that his fracture "involved both parietal bones, measuring one-half by one inch, the longest diameter running at right angles with the sagittal suture."25 Such differences stemmed, in part, from the well-known fact that the prewar education of Civil War surgeons itself was far from standardized and ran from informal apprenticeship to a practicing doctor to years spent observing British and European master surgeons at work.26 The inexperienced and uneducated lacked the language needed for precise anatomical and pathological descriptions.
Certainly some practitioners relished the opportunity to gain experience wielding surgical instruments by performing autopsies, and some were undoubtedly anxious to learn the technical language needed to communicate their observations most effectively. Others simply lacked the time, the interest, or the stomach to open up the dead. Army surgeons had to complete the paperwork to keep track of the sick and wounded, but the surgeon generals never directly ordered all surgeons to perform autopsies and make detailed notes, as much as they might have wished they could.27 The postmortem reports that follow some patients' stories after death thus speak to the degree to which the desire for self-improvement or the duty to contribute to the stockpile of medical knowledge motivated doctors in the field and in the hospital.
Interwoven into autopsy accounts are references to physical specimens gathered and sent to Washington for deposit in the Army Medical Museum. The museum housed the material relics of the doctors' war: parts removed during operations and autopsies that were collected for further scientific study. Surgeon General Hammond established the Army Medical Museum in 1862 specifically as a repository for the war's pathological bounty, and he called upon all surgeons to forward specimens, with their associated case reports, to Washington.28 As Lenore Barbian, Paul Sledzik, and Jeffrey Reznick have discussed in detail, the human remains from the Civil War have carried multiple identities since the war itself. They were, and are, simultaneously objects of science, of museum curation, and of war memorialization.29 They exist quite apart from the cases that the editors of the MSHWR constructed, and yet are intimately connected to them through the published documentation of the objects' retrieval during the war. "The pathological specimen was sent to the Army Medical Museum," noted the editor of Ethan Crane's case, during which the surgeon removed part of Crane's skull for later study.30 At the time that Crane's MSHWR case was written, that part of his skull was "numbered 1393 in Section I" in the museum, where interested readers could examine it for themselves. The ongoing links between case narratives and their associated physical specimens (many of which still exist in the Armed Forces Institute of Pathology's section of the National Museum of Health and Medicine) embed these MSHWR accounts in a disconcerting extranarrative reality. No matter what historical or literary interpretations these cases may generate, they will always be tethered to nonmetaphorical body parts.
The illustrations that accompany perhaps half of the cases add a different nonverbal element to these narratives. The printed illustrations were reproduced from line drawings, watercolor paintings, and black-and-white photographs. Basic lithographs, because they could be printed within the text, are the most numerous; the color and photographic pictures are limited to interleaved plates. Many of the illustrations depict the pathological specimens extracted from the soldiers' bodies, and so connect the editors' descriptive prose with the items in the Army Medical Museum's collections. Others derive from photographs taken of wounded soldiers for the Army Medical Museum (see the illustration of Private Rush, Figure 2).31
The former are easily interpreted as pictures of objects, but the latter have a more ambivalent status. They are at once portraits of individual soldiers and illustrations of effective surgical procedures. As portraits they individuate; as medical illustrations they generalize. The claim to individual identity brings verisimilitude to the knowledge that the illustration offers: here is a real case of successful double amputation at the midthigh. At the same time, the medical knowledge conveyed is supposed to be generalizable: this illustration merely illustrates a procedure that has been, and will be, successful on other wounded men. This tension is ubiquitous in scientific and medical illustration.

Images of men showing their faces and other identifying attributes have a third purpose in the MSHWR: recognizing those who served and sacrificed. Lt. Col. George R. Maxwell, for example, was wounded on April 1, 1865.32 He entered Armory Square Hospital on April 16 with his left leg in serious condition; it was then amputated at mid-thigh. At some point before his discharge from service on August 8, his photograph was taken. By the time the volume containing his case was published, eighteen years had passed since Maxwell's wounding and the end of the war. Depicting him in uniform may have simply underscored the obvious—that the Surgeon General's Office was making an enormous effort to process the piles of facts about the Civil War's wounds and diseases—but it nevertheless made that point visible in ways that words could not (Figure 3). The editors noted, moreover, that George Maxwell was still receiving a pension for his disability on June 4, 1879. The nation was still paying for the war, both in cash and in hampered lives.

One rare case in the second surgical volume of the MSHWR (1876) provides a useful counterpoint to the thousands of other narratives in the series because it contains a first-person narrative of wounding, hospital care, and recovery. Lt. J. E. Mallet, wounded at Cold Harbor on June 3, 1864, survived the war and, at the time that this volume was composed, held "an important civil office under the Government." He "kindly prepared an account of his case," which, the editor noted, "is peculiarly valuable because of the rarity with which reliable information of the immediate symptoms produced by severe wounds can be obtained." The editor stressed that "the authenticity of the facts is unquestionable," as they corresponded to "the testimony of the medical attendants." Mallet's account dwelt particularly on his wounding and the long travel from the battlefield to Washington. His case was accompanied by an illustration (Figure 4) and a specimen, the conoidal ball with which he was shot.33 "The missile entered my left side," he recalled.
I distinctly remember the sensations experienced upon being hit. I imagined that a cannon-ball had struck me on the left hip-bone, that it took a downward course, tearing the intestines in its course, and lodged against the marrow of the right thigh bone. I fancied I saw sparks of fire, and curtains of cobwebs wet with dew, sparkling in the sun. I heard a monstrous roar as of distant cataracts. I felt my teeth chatter, a rush of blood to my eyes, ears, nose and to the ends of my fingers and toes.
He tried to get up, fell, and "became completely insensible." He described his wait on the battlefield (at least a day) and the journey to the hospital transport ship quite matter-of-factly. Men in his regiment on the ship told him that he was "regarded as a dead man." Upon arrival in Washington, he "asked to be taken to Douglas Hospital" but ended up in Armory Square, where his wound was cared for until he was transported out to a hospital in Oswego, New York. Mallet rarely mentioned his pain, although he acknowledged that he "suffered greatly during the [wound] dressings," and he expressed no disgust at the "foetid discharge" from his wound.

Mallet's laconic description of the weeks in which his wound gradually healed matches the editors' tone in the vast majority of the MSHWR cases. Pain and suffering were mentioned, but Mallet merely acknowledged their existence without trying to describe them in any detail. This absence of evocative words for pain (deep, throbbing, stabbing, penetrating, burning, unrelenting) and its effects (crying, screaming, wishing for death) maintained the stoic character of the soldier, at least in terms of what the editor included within Mallet's published account. As such, Mallet's testimony confirmed (for himself and others) the remarkable strength of the Union man who did not let his suffering mar his courage and fortitude.
Mallet's story diverged from those written by surgeons in two important ways: the attention paid to the wounding itself and the underlying sense of his helplessness between the wounding and the day that he sat up in an armchair for the first time four and a half weeks later. Whoever solicited Mallet's statement may well have asked for "the immediate symptoms produced by severe wounds" in order to satisfy doctors' curiosity about this experience, for it had little significance for medical treatment. Mallet's short but vivid description of the immediate trauma emphasized what he appeared to see and to hear, omitting any mention of fear (except for being trampled by other soldiers) or anxiety about the coming pain and possible death. His helplessness when waiting on the field for retrieval, in the ambulance for transport to the river landing, and on the boat for passage to Washington underscored his sudden and total transformation from a soldier engaged in battle to a patient at the mercy of others. His helplessness was further demonstrated when he asked to be taken to Douglas Hospital, presumably to be with men from his regiment, and his wishes were ignored. The rest of his account was basically about waiting, as the surgeons only interfered with his wound when it was obvious that the parts of his clothing that had been caught in it needed to be removed.
As interesting as Mallet's perspective was for his case, it added no useful medical facts to the record. Indeed, his impression of his injury (that a ball seemed to hit his left hip, that the ball ended up in the right thigh) differed from what the doctors knew (the ball entered his abdomen and exited his back). Mallet's mistake nicely illustrated the triumph of expert observation over the value of the patient's immediate awareness of his own condition. The very absence of patients' accounts of their diseases and injuries in the vast majority of cases thus repeatedly demonstrated that doctors made medical knowledge; patients just made medical data.
As clearly constructed as the cases in the MSHWR are, they are nevertheless vital sources for grasping the wounds and diseases that characterized the doctors' Civil War. They document the enormous effort that the surgeon general's staff faced when trying to make sense of the data that deluged them during, and immediately after, the war. The authors of these volumes worked hard to discern meaningful generalizations from this wealth of material, and much of the text of five of the volumes was devoted to discussing relevant medical literature and summarizing their data. Yet page after page was devoted to recounting individual cases, as if the authors could not bear to smooth out the facts of distinct clinical encounters or to entirely separate the data from the identities of the soldiers whose names they recorded. To read these cases is to witness an unsuccessful struggle to create dispassionate science out of the raw stuff of life.
Crossover: L'Ouverture Cases in the MSHWR
To compare the cases in the L'Ouverture Hospital register with those in the MSHWR is to compare raw data points with constructed narratives. Thirty MSHWR cases in the Civil War Washington collection named soldiers who had been patients at L'Ouverture.34 All but one name appears in the hospital register.35 Of the surgical cases discussed, Pvt. Joseph Freeland's case is particularly useful for illustrating the relationship between the register and the MSHWR. Freeland's name appeared in the L'Ouverture register on August 9, 1864. Age 18, Freeland served in Company A of the Thirtieth Regiment USCT. He entered from a field hospital with a gunshot wound to the head. No other columns were filled in, except for his date of discharge from the army on June 8, 1865. The narrative about his case in the MSHWR provides details and discrepancies.36 In that text, Private Freeland was wounded from a shell, not a gunshot, that fractured his skull on July 10, 1864. A regimental surgeon, David Mackay (29th USCT), "trephined the skull, and removed one and one-fourth inches of right parietal bone, while the patient was under the influence of chloroform." Freeland was moved to a staging hospital at City Point, Virginia, and moved on to Alexandria five days later. The MSHWR account included the fact that "his left arm and leg were paralyzed." It is tempting to assume that the MSHWR account was more accurate simply because there was more of it, but without knowing what Surgeon MacKay's notes contained, to do so would be unwise. Whether by gunshot or shell wound, this 18-year-old ended up with a "total and permanent" disability.
The case of William Lewis, a civilian, leads us to other insights about these sources. The register has William Lewis entering on May 19, 1864, from Alexandria, with a diagnosis of "inflammation of the lungs" and dying on October 4, 1864, with no cause of death recorded. The MSHWR case in contrast provided his age (28) and an entering diagnosis of pneumonia (essentially inflammation of the lungs).37 The case became more complicated in August, when it was noted that he "was suffering from ascites," or an accumulation of fluid in his abdomen, with swelling of his legs. Acting Assistant Surgeon W. K. Fletcher, who apparently recorded notes on the case, described Lewis's treatment and ultimate death. The postmortem showed abscesses in the liver and "a cavity filled with pus" in the spleen. The register—to make this point again—clearly contains Lewis's initial diagnosis and acknowledges his death. The MSHWR case—again—reveals that at some time during or after the war, Fletcher submitted his case notes to the Surgeon General's Office. Those notes included the postmortem observations, the focus of which suggests Lewis died not of pneumonia but of inflammation and infection in his abdominal organs, although that was never stated explicitly.
None of the notes in the hospital register indicated which bodies were autopsied of the 279 known to have died there or even that autopsies were performed at all. In contrast, of the 29 L'Ouverture Hospital cases in the MSHWR, surgeons autopsied all of the 25 men who died. Whether that autopsy rate is at all typical remains an open question for further study of Civil War hospital registers and MSHWR texts. It raises the possibility, nevertheless, that postmortem examinations of African American bodies were done with more than usual frequency. As has been explained elsewhere, from 1862 on the Surgeon General's Office had made it a policy to keep the data on black soldiers separate from that for white soldiers, so that racial differences and similarities could be studied after the war.38 It is also quite possible that northern surgeons assigned to L'Ouverture simply chose to satisfy their curiously about the black bodies that the war provided.
Comparing one register and MSHWR entries can only suggest the ways that examining cases recorded at one moment may lead to different conclusions than studying them from a postwar vantage point. Putting them side by side nevertheless underscores how the doctors experienced medical practice and medical knowledge during the war. In those years, the goal was largely to take down the records, to write the reports, and to compile the paperwork, with very little time to grasp what it all meant. So, too, the historian must remember that the words jotted in hospital registers were transitory truths, subject to the changing conditions of the very bodies they referred to. The postwar narratives, in turn, primarily depended upon surgeons' wartime accounts, in whatever myriad ways these were written at the time, and they may or may not be consistent with what we find in the registers. To expect otherwise is to expect that the experience of the war itself must have had coherence and to forget that such coherence could only have been constructed after the war was over.
Conclusion
The military required that soldiers be accounted for, from mustering to death or discharge. The surgeons to regiments, field hospitals, and general hospitals took responsibility for keeping track of soldiers' bodies. Expectations about the need to document medical discharges and reasons for postwar pensions meant that at least a minimal record had to be kept of a sick or wounded soldier's condition. Thus the paperwork accumulated. At the same time, the military offered army surgeons an unprecedented opportunity to observe, control, treat, and autopsy the soldiers who came into their care. The surgeon general's pleas to keep case notes, write reports, and submit pathological specimens added a duty to contribute to the vast stockpile of data that would become medical knowledge after the war, although certainly not all military surgeons were able or willing to join these efforts.
To read cases in hospital registers and from the MSHWR is to enter very different medical worlds, albeit worlds that touched briefly. The former offer the immediacy of primary archival sources, while the later present constructed narratives. The former certainly are more complete, in that doctors attempted to record all of the civilians and soldiers who occupied beds in their institutions. In contrast, the editors of the MSHWR selected the case narratives to include in their volumes. They chose cases that illustrated the more general observations that they made in the text from all of those for which they had surgeons' notes to supplement the terse entries found in regimental or hospital registers, although they undoubtedly used some of those as well. Since only the more dedicated practitioners even made case notes, the MSHWR cases hardly form a random sample. For all of their flaws, nevertheless, the MSHWR cases, along with entries in field and hospital registers, bring us as close as we are ever likely to get to the doctors' war.
Notes
This essay was first published in Civil War Washington: History, Place, and Digital Scholarship, ed. Susan C. Lawrence (Lincoln: University of Nebraska Press, 2015). It is reproduced with permission and has been revised and updated for publication here, as described in "Civil War Washington: The City and the Site." The copyright to this essay is held by the Board of Regents of the University of Nebraska, and Civil War Washington's Creative Commons license does not apply to it.
- The total number of cases counted in the MSHWR comes from adding the total number of white cases to the total number of black cases in the summary tables in pt. 1, v. 1, pp. 641 and 712. While these were individual medical events, soldiers certainly experienced more than one illness, even more than one injury, throughout their terms of service. These are just the cases, moreover, for which some record was made in a form that could be evaluated by the Surgeon General's Office after the war. [back]
- Military pension records for civil war soldiers provide yet another collection of cases for study. The Center for Population Economics at the University of Chicago has taken a sample of pensions for approximately 39,000 white male soldiers, with linked data from surgeon's certificates and from the federal census records. There is a similar sampled set of Union African American troops. These anonymized data sets are available for download from http://research.chicagobooth.edu/cpe/. The Center will release sets with names only for special research projects. NARA has embarked on a plan to digitize all pension files. [back]
- The L'Ouverture Hospital register is clearly a fair copy made of an earlier volume. Such transcription was a source of an obviously unknown number of errors. The register is located in the National Archives and Records Administration, RG 94, Field Records of Hospitals, 1821–1912, Register 578. [back]
- Three other hospitals were run by the military for African Americans during the war. The Freedmen's Hospital served contrabands and other civilians in Washington. Its records appear to be lost, as they are listed neither at the National Archives nor at Howard University. The Claremont Smallpox Hospital, created on the outskirts of the District, opened in November or December 1862. Black civilians in Alexandria and both black and white soldiers were sent there in attempts to contain smallpox, which regularly broke out in Alexandria. See Tim Dennee and the Friends of the Freedmen's Cemetery, "African-American Civilians and Soldiers Treated at Claremont Smallpox Hospital, Fairfax County, Virginia, 1862–1865" (2008, 2010, 2011) online article at http://freedmenscemetery.org/resources/documents/claremont.pdf (accessed November 6, 2012). The military director of Alexandria, General Slough, allocated a house to Dr. John Bigelow in January 1863 to serve as a hospital for contrabands. Tim Dennee and the Friends of the Freedmen's Cemetery, "A House Divided Still Stands: The Contraband Hospital and Alexandria's Freedmen's Aid Workers" (2011) online article at http://www.freedmenscemetery.org/resources/documents/contrabandhospital.pdf (accessed November 7, 2012). [back]
- Dennee, "A House Divided Still Stands." [back]
- Dennee, "A House Divided Still Stands." [back]
- L'Ouverture had an official capacity of 500 by July of 1864 and an official maximum of 692 in March 1865. See RG 94 Records of General Hospitals. The total number of entries in the register was 1,648, but at least 65 of these were the same men returning after being away on furlough, desertion, or (for one civilian) repeat visits. The total number used in our calculations was thus 1,583. [back]
- Margaret Humphreys, Intensely Human: The Health of the Black Soldier in the American Civil War (Baltimore: Johns Hopkins University Press, 2008). [back]
- For details on the petitions filed under the Compensated Emancipation Act of April 1862, see Kenneth J. Winkle, "Emancipation in the District of Columbia" and "Mining the Compensated Emancipation Petitions." [back]
- Walt Whitman, Memoranda of the War (Camden NJ: 1875–76), 3, 10, 55–56. See also Specimen Days in the Complete Prose Works (Philadelphia: David McKay, 1892) for a further collection of Whitman's pieces about the war. An important contribution to this discussion is Lenore Barbian, Paul S. Sledzik, and Jeffrey S. Reznick, "Remains of War: Walt Whit-man, Civil War Soldiers, and the Legacy of Medical Collections," Museum History Journal 5 (2012): 7–28. [back]
- Susan C. Lawrence, "Medical and Surgical Cases: Sources and Methods." Barbian, Sledzik, and Reznick, "Remains of War" provide examples of the relationship between case notes (at least those that survive) and the narratives in the MSHWR for four patients that Whitman cared for, and so confirm that the MSHWR's editors selected cases to include in order to serve the purposes of their larger discussions of wounds and diseases. [back]
- John Harley Warner, The Therapeutic Perspective: Medical Practice, Knowledge, and Identity in America, 1820–1885 (Cambridge: Harvard University Press, 1986). [back]
- While several of the key foundations for bacteriology were laid in the 1860s and 1870s, including the idea that infection-causing bacteria should be killed with strong antiseptics applied to wounds and operative fields, the acceptance of this new science and what it entailed for medical and surgical practice took decades. See William Derek Foster, A History of Medical Bacteriology and Immunology (London: Heinemann Medical, 1970); Nancy Tomes, The Gospel of Germs: Men, Women, and the Microbe in American Life (Cambridge: Harvard University Press, 1999); Anna Greenwood, "Lawson Tait and Opposition to Germ Theory: Defining Science and Surgical Practice," Journal of the History of Medicine and Allied Sciences 53 (1998): 99–131. [back]
- William Ells; Print: MSHWR, pt. 1, v. 2 (Washington DC: Government Printing Office, 1870), 6. [back]
- On the web page for the Ells case (note 14), click on "incised scalp wounds" in the Keywords field. The search will return fifty-three results, all uneventful cases. [back]
- William Nims; Print: MSHWR, pt. 1, v. 2, 329–30; Steven M. Stowe, "Seeing Themselves at Work: Physicians and the Case Narrative in the Mid-Nineteenth-Century American South," American Historical Review 101 (1996): 41–79. For an analysis of this genre in eighteenth-century medical literature, see Susan C. Lawrence, Charitable Knowledge: Hospital Pupils and Practitioners in Eighteenth-Century London (New York: Cambridge University Press, 1996). [back]
- John Lower; Print: MSHWR, pt. 3, v. 1 (Washington DC: Government Printing Office, 1888), 776. [back]
- Only smallpox had been proved to be passed from person to person by some substance produced in the body and not caused by an environmental influence. [back]
- John Harley Warner, Against the Spirit of System: The French Impulse in Nineteenth-Century American Medicine (Baltimore: Johns Hopkins University Press, 2003). [back]
- For an example of a case where a diagnosis of typhoid was not confirmed at autopsy, see John Shay; Print: MSHWR, pt. 3, v. 1, 767. [back]
- The entire second medical volume (1876) was devoted to the diseases that presented with diarrhea and dysentery. [back]
- See, for example, the case of William Brandt; Print: MSHWR, pt. 3, v. 1, 352. [back]
- Using the search box on the Texts page, search for "postmortem" and "autopsy" to see the range of observations made on patients after death. These form the basis for the conclusions made in this discussion. [back]
- Henry Clark; Print: MSHWR, pt. 1, v. 2, 258. [back]
- Otis G—; Print MSHWR, pt. 1, v. 2, 248–49. [back]
- James H. Cassedy, Medicine in America: A Short History (Baltimore: Johns Hopkins University Press, 1991). [back]
- See the prefatory collection of official War Department letters circulated to all surgeons, MSHWR, pt. 1, v. 2, 1870 (the first surgical volume). These memoranda outline the reports that the medical directors were required to forward to the Surgeon General's Office, including changes in the format of reporting forms and registers from 1863 and 1864. [back]
- Prefatory, MSHWR, pt. 1, v. 2, vi–vii. [back]
- The collections of the nineteenth-century Army Medical Museum are now housed in the National Museum of Health and Medicine (www.medicalmuseum.mil). See Barbian, Sledzik, and Reznick, "Remains of War," 7–28. [back]
- Ethan Crane; Print: MSHWR, pt. 1, v. 2, 112. [back]
- MSHWR, pt. 3, v. 2, 243. [back]
- MSHWR, pt. 3, v. 2, 278.[back]
- MSHWR, pt. 2, v. 2, 90–91. [back]
- Enter "L'Ouverture" in the search box on the Texts page for a full list of the cases in the MSHWR.[back]
- Horace Hill appears in the MSHWR as having been a patient in L'Ouverture Hospital, but is not in the hospital register. Since the MSHWR text says that he was admitted on November 7, 1865, and the hospital was closed by then, his status as a patient remains puzzling; Print: MSHWR, pt. 3, v. 1, 132. [back]
- Joseph Freeland; Print: MSHWR, pt. 1, v. 2, 290. [back]
- William Lewis; Print: MSHWR, pt. 3, v. 1, 878. [back]
- Susan C. Lawrence, "Medical and Surgical Cases: Sources and Methods." [back]